“I’m so OCD”. If I had a dollar for how many times I’ve heard that phrase (and once seen it embroidered onto a cushion), I’d have quite a few dollars.
Maybe not up to Elon Musk level, but at least former-Neighbours-star type wealth.
The contexts in which I’ve heard that phrase most often are: people who get a kick out of lining up their coloured pens, anyone who loves kikki.k and people who don’t have a Laundry Chair.
Well, I have OCD and I’m here to tell you: that’s just called being an earth sign.
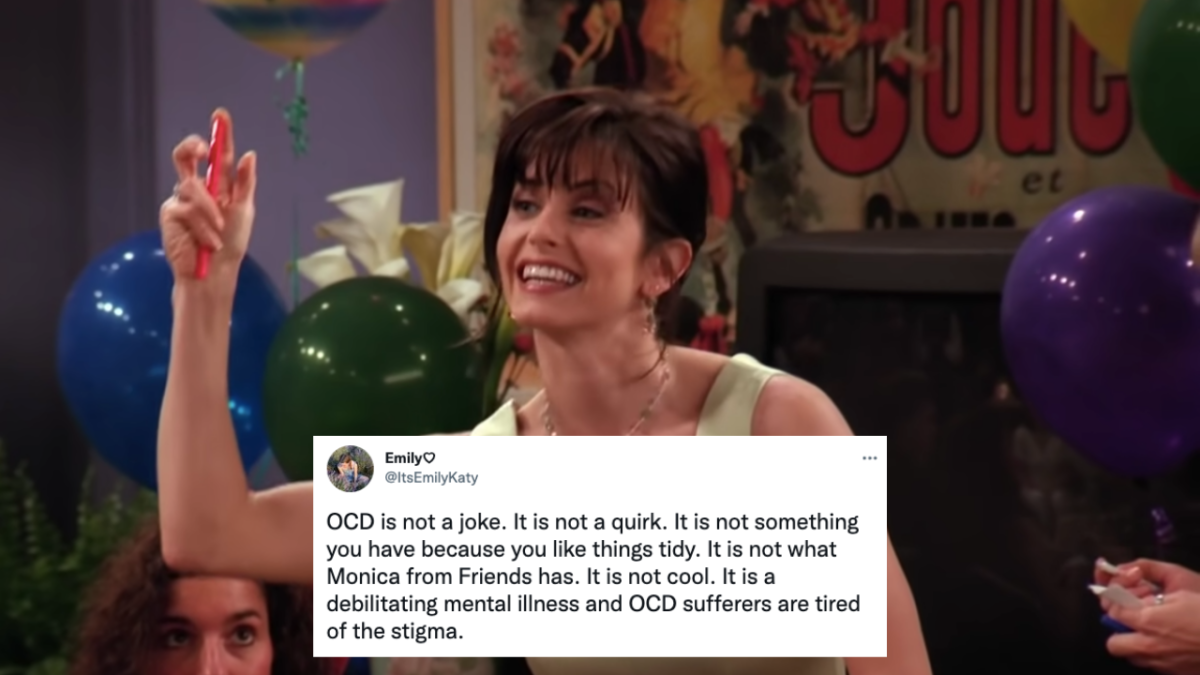
We’ve had a big cultural shift in the last few years, opening up conversations about mental illness and neurodivergence. But there are still massive misconceptions around OCD and what living with it is really like.
According to Health Direct, more than 500,000 Aussies have OCD. So why don’t we understand it better?
What do people think of when they think about OCD?
If you had asked me to tell you what OCD was three years ago, I probably would’ve told you it was when people are scared of germs. While contamination obsessions are common, they’re definitely not the whole story of OCD.
Surprise! It’s a War And Peace length novel.
Part of the reason it took so long for me to realise I had OCD was because I don’t really care about cleanliness (not in a gross way, I promise). But I’m a firm believer in the 5-second rule, my bedroom is constantly messy and while I’m a hypochondriac, my anxieties around health didn’t start until after the pandemic hit. Thanks again, COVID.
Plus, I did a Year 11 psychology class where we literally studied OCD! And I still thought it was all about handwashing! Blaming that one on the SACE board, TBH.
Dr David Berle, a clinical psychologist with at the University of Technology Sydney told PEDESTRIAN.TV that labelling your quirks or habit as being “a bit OCD” can produce stigma.
“We don’t make jokes about being a “little depressed” as if it’s an endearing or productive trait, so I think making light of OCD can sometimes undermine the very real challenges and distress experienced by people with severe OCD,” he explained.
“OCD affects people in very different ways, but as an example, if you can imagine how tormenting it would be to live with the constant fear that if you didn’t perform a particular ritual, a loved one might die [or] your house might burn down.
“That is the sort of distress that many people with OCD have to live with every day.”
So what’s the real deal?
OCD was initially categorised as an anxiety disorder, but it’s since been categorised as its own seperate disorder.
Living with OCD falls into two parts: obsessions and compulsions.
Obsessions are intrusive thoughts. For me, it’s like my brain gets stuck on the worst possible thing it can imagine.
That could range from obsessing over whether you left the oven on to intrusive thoughts of you violently harming someone you love.
The list of intrusive thoughts that many people with OCD suffer from are uncomfortable. When you have undiagnosed OCD and you don’t know what intrusive thoughts are, they can be incredibly scary. You’re walking down the street and seemingly out of nowhere, an incredibly uncomfortable sexual or violent thought pops into your brain.
You don’t understand why you’re thinking about this terrible thing, which can have a massive impact on your sense of self.
“The interesting thing about obsessions is that for someone with OCD, the most upsetting obsessions tend to be about things that they are unlikely to ever intentionally act on (e.g. harming their child in some way),” said Dr Berle.
“But the thought of it terrifies them so much that they feel overwhelmed by it.”
Compulsions are behaviours: the things that OCD sufferers perform to try and deal with obsessions. For example, someone who has intrusive thoughts about contamination might try and ease that thought by compulsively washing their hands.
Other common compulsions including hair and skin picking, hoarding or checking (where you continually check taps, locks and light switches).
View this post on Instagram
“People with OCD can find themselves in a trap where they feel highly distressed by an obsessional thought and feel that the only thing that relieves it is performing a particular compulsion,” explained Dr Berle.
Spoiler alert! Performing compulsions actually don’t make you feel better.
“Performing compulsions typically only provides brief relief from the distress,” Dr Berle said.
“Because the obsessional thoughts keep arising, the person can end up feeling stuck in an endless cycle.”
That sounds pretty shite, TBH.
I’m a 23-year-old who’s lived out of home since I was 18. Over the course of those five years, I’ve been through multiple periods of having to double check in my wardrobe before bed.
Why you ask? Because of a recurring intrusive thought that someone could be hiding in my wardrobe waiting to hurt me. Is it logical? No! Could a human person fit in my two-door IKEA wardrobe? No! Well, maybe a murderous contortionist.
Is it embarrassing to tell people I have to check for monsters in my wardrobe as an adult? Well, yes.
But that’s a reality of living with OCD: you know your obsessions are not necessarily logical.
“By its very nature, OCD leaves [people] feeling unable to tolerate even the smallest possibility that their doubts may eventuate,” said Dr Berle.
Hence multiple times where I’ve missed buses, run late for social events and even shown up late for work because I had to walk 10 minutes back to my house to double check I locked the front door or turned off the oven.
Before I realised I had OCD, there were periods where I’d spend dawn to dusk just desperately trying to shut out my intrusive thoughts. But because my view of OCD was hand-washing and colour coordination, I had no idea what was happening to me. I genuinely just thought I was a terrible person.
How is OCD treated?
I’d suspected I had OCD for about a year before I went to my GP to get a mental health plan. It took a lot of my own research and a friend being diagnosed with OCD for me to realise what I was struggling with.
Usually, OCD is diagnosed by a psychiatrist or a clinical psychologist. They’ll do a background interview and try to suss out if there are any other explanations for the symptoms.
Sometimes people with OCD are prescribed anti-depressants. A form of Cognitive Behavioural Therapy (CBT) called Exposure and Response Prevention (ERP) is also a popular way of treating it.
“[This] involves the person systematically exposing themselves to the obsessional thought or doubt but resisting engaging in the associated compulsion,” said Dr Berle.
According to Dr Berle, while ERP can be really intense it has also been found to be effective.
So, your well organised kitchen cupboard and wardrobe aren’t necessarily signs of OCD and they shouldn’t be treated as such.
Phrases like “I’m a little OCD” cloud our understanding of what living with OCD is really like and can make it harder for sufferers to realise what they’re struggling with.
Personally? I reckon we all just start saying we’re in our Virgo era instead.